
By Kate Lange, MPH; Eileen Partridge, DNP, AGPCNP-BC; and Cynthia Carlsson, MD, MS
Hypertension is the leading risk factor for disability and premature death worldwide (Lim et al., 2012). High blood pressure can result in the complications of heart disease, heart failure, stroke, peripheral arterial disease, kidney disease, retinopathy, and death. In 2005, high blood pressure was associated with one of every six preventable deaths in the United States (Danaie et al., 2009). This modifiable risk factor affects nearly half of American adults and has a prevalence of over 75% in adults aged 65 and older (ACC/AHA Task Force Task Force on Clinical Practice Guidelines, 2017).
In 2017, new guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA) changed how we approach treatment of high blood pressure in older adults, lowering the threshold for treatment and goal blood pressure (BP) for adults. This change was based in large part on results from the Systolic Blood Pressure Intervention Trial (SPRINT). SPRINT (Wright et al., 2015 and Williamson et al., 2016) compared the benefits of treating systolic BP to a target of less than 120 mmHg to the standard target of less than 140 mmHg. The trial was terminated early due to findings that adults (including those over age 75 years) treated to the lower BP goal had lower rates of cardiovascular events and death.
In early 2019, investigators published additional findings from the Memory and Cognition in Decreased Hypertension (MIND) component of SPRINT. This sub-study, completed among adults over the age of 50, compared the effect on cognition when treating hypertension with an intensive systolic blood pressure goal of 120 mmHg compared to standard care, finding that intensive treatment significantly reduced the risk of mild cognitive impairment (MCI) and the combined outcome of MCI or dementia. SPRINT-MIND was the first randomized controlled trial to demonstrate an intervention to reduce risk of MCI, reinforcing the importance of hypertension management in older populations.
Given the finding of the SPRINT trial and the direct impact on standards for care for older adults with hypertension, we will describe the major changes in hypertension management guidelines and discuss the implications of the SPRINT-MIND findings.
Changes in 2017 guidelines
The release of the 2017 ACC/AHA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults updated the 2003 guideline released by the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). The Joint National Committee also published guidelines for the management of hypertension (HTN) in 2014 – known as JNC 8 – however in 2013, the National Heart, Lung, and Blood Institute had asked the ACC & AHA to assume responsibility for cardiovascular disease prevention guidelines (Gibbons et al., 2013). Therefore, the focus on updated guidelines is based off the 2017 ACC/AHA guidelines.
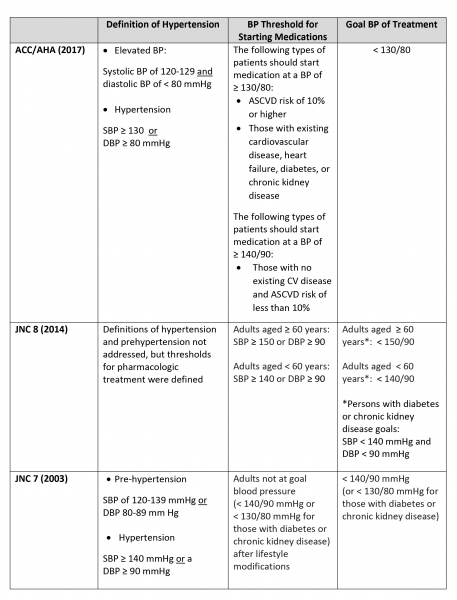
The 2017 ACC/AHA update lowered the threshold for treatment and BP goals of adults compared to JNC 7 and JNC 8 guidelines. Due to SPRINT results, the 2017 ACC/AHA guidelines are applicable to all adults, including adults over the age of 65. In addition to establishing lower thresholds, the ACC/AHA update recommends that providers use the 10-year calculated atherosclerotic cardiovascular disease (ASCVD) risk for patients to decide whether to start patients on BP-lowering medications, which was not previously recommended by JNC 7 or 8. Lifestyle changes are recommended across all guidelines. The table below compares the 2017 ACC/AHA BP thresholds with JNC 7 and 8 for the general population:
At the time of the release of the JNC 8 guidelines, the recommendations for treating older adults to a goal of 150/90 were based on lower quality evidence that a goal systolic BP lower than 140 mmHg for adults over the age of 60 did not provide additional benefits. The SPRINT trial brought forth evidence that more intensive BP treatment, with a target systolic BP of less than 120 mmHg, significantly reduced cardiovascular events and mortality. In SPRINT participants over the age of 75, more intensive BP treatment reduced cardiovascular events and mortality was reduced by approximately 33% (Williamson, Supiano, et al., 2016).
SPRINT also addressed some of the concerns related to bringing down blood pressure more intensively in older adults. Those that were treated to a lower BP goal did have more occurrences of hypotension, syncope, electrolyte abnormalities, and acute kidney injuries, but these rates were not statistically significantly different than the standard treatment arm. Falls leading to injury were lower but not statistically significantly different in the intensive treatment group. Due to the possible adverse outcomes, current ACC/AHA guidelines specify that for adults over the age of 65, clinicians should exercise judgement, discuss patient preferences, and use a team approach for decisions on a BP goal and on pharmacological treatment.
Blood pressure management and cognitive decline
The SPRINT-MIND sub-study primarily focused on whether intensive BP management lowered the risk of probable dementia. Over a 5 year follow-up period, investigators did not find a statistically significant reduction in probable dementia but did find that treating patients to a lower systolic BP goal of 120 lowered the risk of mild cognitive impairment (MCI) and the combined rate of probable dementia and MCI. As a stage in the Alzheimer’s disease continuum, approximately 10% of people with MCI progress to dementia annually, but not all people with MCI will progress along this continuum. Intensive blood pressure control lowers the risk of developing MCI, but the impact on rates of dementia or the progression of MCI to dementia are not clear.
The 2017 guidelines for the management of HTN did not outline specific blood pressure goals for patients with MCI or dementia. However, the ACC/AHA recommended that in adults with hypertension, lowering BP is reasonable in order to prevent cognitive decline. The SPRINT-MIND results, which came out after the 2017 guidelines, have no doubt strengthened that recommendation.
References
Chobanian, A. V., Bakris, G. L., Black, H. R., Cushman, W. C., Green, L. A., Izzo Jr, J. L., ... & Roccella, E. J. (2003). The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama, 289(19), 2560-2571.
Danaei, G., Ding, E. L., Mozaffarian, D., Taylor, B., Rehm, J., Murray, C. J. L., & Ezzati, M. (2009). The Preventable Causes of Death in the United States: Comparative Risk Assessment of Dietary, Lifestyle, and Metabolic Risk Factors. PLOS Medicine, 6(4), e1000058. https://doi.org/10.1371/journal.pmed.1000058
Gibbons, G. H., Harold, J. G., Jessup, M., Robertson, R. M., & Oetgen, W. J. (2013). The Next Steps in Developing Clinical Practice Guidelines for Prevention. Journal of the American College of Cardiology, 62(15), 1399–1400. https://doi.org/10.1016/j.jacc.2013.08.004
James, P. A., Oparil, S., Carter, B. L., Cushman, W. C., Dennison-Himmelfarb, C., Handler, J., Lackland, D. T., LeFevre, M. L., MacKenzie, T. D., Ogedegbe, O., Smith, S. C., Svetkey, L. P., Taler, S. J., Townsend, R. R., Wright, J. T., Narva, A. S., & Ortiz, E. (2014). 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA, 311(5), 507–520. https://doi.org/10.1001/jama.2013.284427
Lim, S. S., Vos, T., Flaxman, A. D., Danaei, G., Shibuya, K., Adair-Rohani, H., Amann, M., Anderson, H. R., Andrews, K. G., Aryee, M., Atkinson, C., Bacchus, L. J., Bahalim, A. N., Balakrishnan, K., Balmes, J., Barker-Collo, S., Baxter, A., Bell, M. L., Blore, J. D., … Ezzati, M. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380(9859), 2224–2260. https://doi.org/10.1016/S0140-6736(12)61766-8
The SPRINT MIND Investigators for the SPRINT Research Group. (2019). Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA, 321(6): 553-561. doi:10.1001/jama.2018.21442
Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., Collins, K. J., Dennison Himmelfarb, C., DePalma, S. M., Gidding, S., Jamerson, K. A., Jones, D. W., MacLaughlin, E. J., Muntner, P., Ovbiagele, B., Smith, S. C., Spencer, C. C., Stafford, R. S., Taler, S. J., Thomas, R. J., Williams, K. A., … Wright, J. T. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension, 71(6), 1269–1324. https://doi.org/10.1161/HYP.0000000000000066
Williamson, J. D., Supiano, M. A., Applegate, W. B., Berlowitz, D. R., Campbell, R. C., Chertow, G. M., Fine, L. J., Haley, W. E., Hawfield, A. T., Ix, J. H., Kitzman, D. W., Kostis, J. B., Krousel-Wood, M. A., Launer, L. J., Oparil, S., Rodriguez, C. J., Roumie, C. L., Shorr, R. I., Sink, K. M., Wadley, V G., … Pajewski, N.M. (2016). Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged ≥75 Years: A Randomized Clinical Trial. JAMA, 315(24), 2673-2682. https://doi.org/10.1001/jama.2016.7050
Wright, J. T. Jr, Williamson, J. D., Whelton, P. K., Snyder, J. K., Sink, K. M., Rocco, M. V., Reboussin, D. M., Rahman, M., Oparil, S., Lewis, C. E., Kimmel, P. L., Johnson, K. C., Goff, D. C. Jr, Fine, L. J., Cutler, J. A., Cushman, W. C., Cheung, A. K., Ambrosius, W. T. (2015). A Randomized Trial of Intensive versus Standard Blood-Pressure Control. New England Journal of Medicine, 373(22), 2103–2116. https://doi.org/10.1056/NEJMoa1511939
- Log in to post comments



